Diabetic neuropathy is a prevalent and serious complication of diabetes that affects millions of people around the globe. This condition results from prolonged high blood sugar levels that damage the nerves throughout the body, causing pain, discomfort, and other debilitating symptoms. Early detection, intervention, and careful management are essential to prevent more severe outcomes. At SimpleeKare Hospital, we aim to provide clear, actionable insights on the symptoms, causes, types, and treatment options for diabetic neuropathy to help you better manage your health.
What is Diabetic Neuropathy?
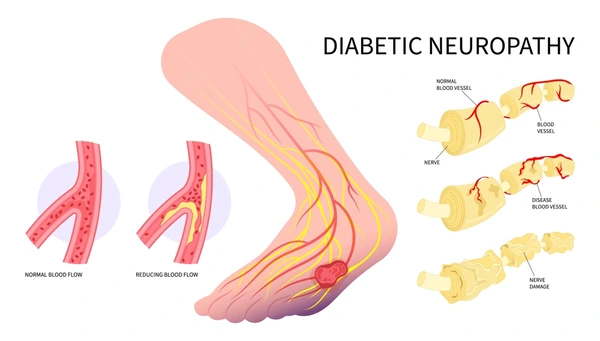
Diabetic-related neuropathy refers to nerve damage that occurs due to long-term exposure to elevated blood glucose levels. This condition can affect a wide range of bodily functions, from basic motor skills to more critical functions like digestion and heart rate. Prolonged hyperglycemia (high blood sugar) damages the nerve fibers, preventing them from transmitting signals properly. Without intervention, diabetic neuropathy can result in irreversible nerve damage, severe pain, and complications that severely impact one’s quality of life.
Symptoms of Diabetic Neuropathy
The symptoms of diabetic neuropathy vary depending on which nerve groups are affected. Common signs include:
- Tingling or burning sensations: Especially in the hands and feet, a common indicator of sensory neuropathy.
- Sharp, jabbing pain: Can be felt in the legs, arms, or feet, and may worsen at night.
- Loss of sensation: This is particularly problematic in the feet, where it may lead to unnoticed injuries or ulcers.
- Weakness in muscles: This can affect the legs and hands, leading to difficulty walking or performing tasks.
- Digestive issues: Nausea, vomiting, and diarrhea can result from autonomic neuropathy.
- Cardiovascular complications: Changes in heart rate or blood pressure can occur, leading to dizziness or fainting.
If you experience any of these symptoms, it is vital to consult a diabetic neuropathy specialist immediately to begin early management.
Causes of Diabetic Neuropathy
The primary factor behind diabetic neuropathy is long-term high blood sugar levels. Over time, excess glucose damages the blood vessels that supply nerves with oxygen and nutrients, leading to nerve degeneration. Other factors that can contribute to the development of neuropathy include:
- Poor blood sugar control: If blood sugar levels are not well-managed, the risk of nerve damage increases.
- High blood pressure: Elevated blood pressure can cause damage to the blood vessels, exacerbating nerve problems.
- High cholesterol: Similar to high blood pressure, high cholesterol can impede proper circulation, worsening neuropathy.
- Smoking: Smoking reduces blood flow, which can exacerbate nerve damage.
- Genetic predisposition: A family history of diabetes or neuropathy may increase your risk of developing the condition.
Addressing these factors can significantly reduce the likelihood of developing diabetic neuropathy.
Types of Diabetic Neuropathy
Diabetic neuropathy can be categorized into four distinct types, each with unique effects on different parts of the body:
- Peripheral Neuropathy: The most common form, it affects the feet and legs first, followed by the hands and arms. It leads to pain, numbness, and weakness in the extremities.
- Autonomic Neuropathy: This type affects the autonomic nervous system, which controls involuntary functions such as heart rate, digestion, and bladder control. It can lead to symptoms like nausea, digestive disturbances, and issues with heart rate regulation.
- Proximal Neuropathy: Typically affecting the hips, thighs, or buttocks, this form causes severe pain and muscle weakness. Proximal neuropathy often starts with pain or weakness on one side of the body but can eventually affect both sides.
- Focal Neuropathy: Involves specific nerves, often in the head, torso, or legs. This type can lead to sudden weakness or pain, and it can come on abruptly.
Understanding the type of neuropathy you have is crucial for determining the appropriate treatment strategy.
Diabetic Neuropathy Treatment
Managing diabetic neuropathy is a multifaceted approach aimed at addressing the underlying causes and alleviating symptoms. Here are some common treatment options:
- Blood Sugar Control: The cornerstone of neuropathy management is keeping blood sugar levels within the target range. Tight blood glucose or diabetes control can slow or even stop the progression of nerve damage.
- Medications: Pain management for diabetic neuropathy often involves medications such as pain relievers, antidepressants (like amitriptyline), anticonvulsants (such as gabapentin), or topical treatments like capsaicin cream.
- Physical Therapy: Engaging in physical therapy can help strengthen muscles, improve coordination, and alleviate discomfort caused by neuropathy.
- Lifestyle Changes: Making dietary adjustments, regular physical activity, quitting smoking, and reducing alcohol consumption can improve overall health and slow the progression of diabetic neuropathy.
- Alternative Therapies: Acupuncture, biofeedback therapy, and even herbal supplements like alpha-lipoic acid have shown promise in managing nerve pain for some individuals.
Best Tips for Managing Diabetic Neuropathy
- Monitor Blood Sugar: Regularly check your blood glucose levels to ensure they remain within the target range.
- Foot Care: Wear comfortable, well-fitting shoes to protect your feet from diabetic foot ulcers or injuries. Regularly check your feet for cuts, blisters, or sores and seek for treatment.
- Exercise: Physical activity improves circulation, nerve health, and muscle strength.
- Regular Checkups: See your diabetic foot ankle specialist near you for regular checkups to track the progression of diabetic neuropathy and adjust treatments as needed.
Simple Ways to Prevent Diabetic Nerve Damage
Preventing diabetic neuropathy is easier than treating it, and there are simple strategies to protect your nerves:
- Manage your blood sugar, blood pressure, and cholesterol: Keep these levels under control to reduce nerve damage risk.
- Maintain a healthy weight: A nutritious diet and exercise routine will help keep you at an optimal weight and reduce strain on your nerves.
- Quit smoking: Smoking reduces circulation and oxygen flow to the nerves, increasing the risk of neuropathy.
- Regular exercise: Exercise improves circulation and helps maintain healthy nerve function.
Expert Advice on Diabetic Neuropathy
A comprehensive approach to managing diabetic neuropathy is crucial for reducing symptoms and improving the quality of life. With professional care, timely interventions, and lifestyle changes, it’s possible to manage and even alleviate many symptoms of diabetic neuropathy. At SimpleeKare, we offer personalized diabetic neuropathy treatment plans designed to help you live pain-free and maintain optimal nerve health. With expert support, you can effectively manage your condition and improve your overall well-being.
For those in need of professional diabetic neuropathy care, be sure to look for diabetic neuropathy treatment near me or inquire about hospital neuropathy services to get timely and personalized care. Taking control of your health and preventing complications can significantly improve your life. For more information on affordable diabetic neuropathy care, Contact SimpleeKare Hospital today.
Leave a Reply