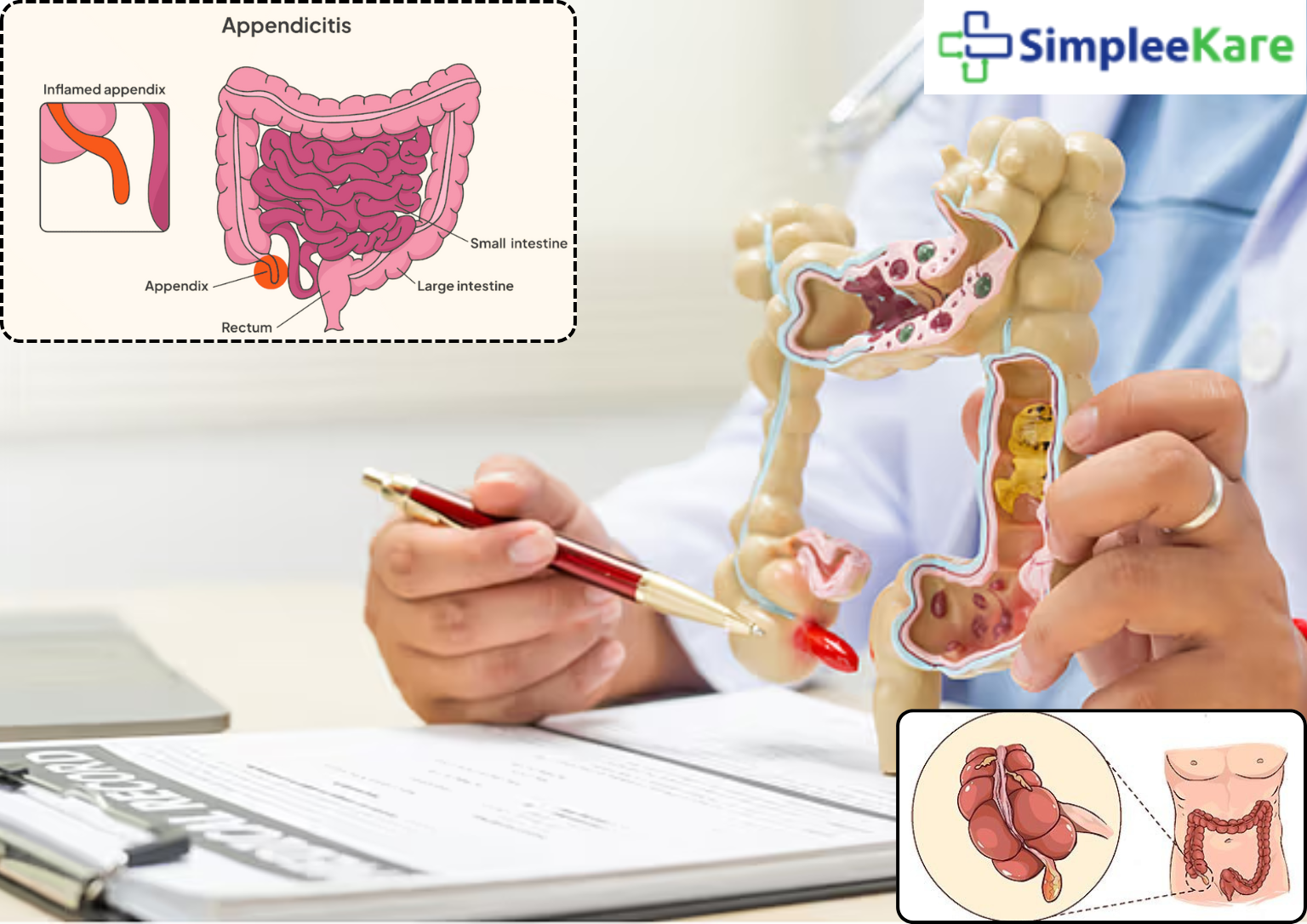
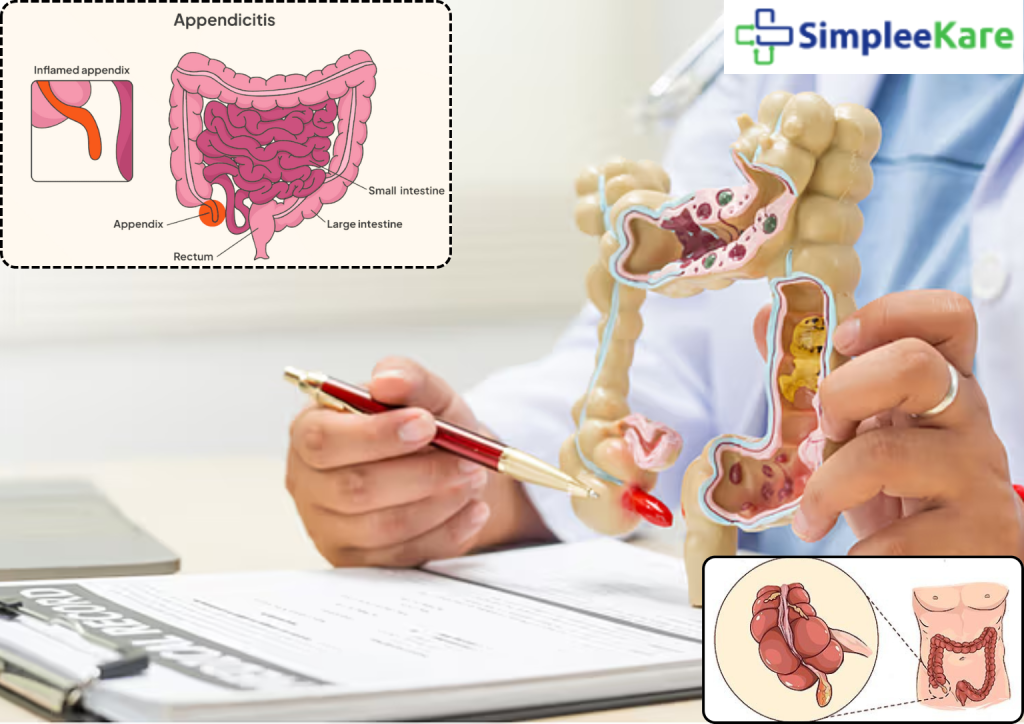
Appendicitis is a medical emergency that occurs when the appendix—a small, tube-like organ attached to the large intestine—becomes inflamed. It is one of the most common causes of sudden abdominal pain that requires surgery. If left untreated, an inflamed appendix can rupture, leading to serious infections and complications. Fortunately, with modern surgical techniques available across India, appendicitis is highly treatable.
What is Appendicitis?
Appendicitis is the inflammation of the appendix, typically caused by a blockage. It can affect people of all ages but is most common in individuals between 10 and 30 years of age. The inflammation can worsen quickly, which is why prompt diagnosis and treatment are essential.
Common Symptoms of Appendicitis
Recognizing the symptoms of appendicitis is crucial for timely treatment. Key signs include:
- Sudden pain starting around the belly button and shifting to the lower right abdomen
- Loss of appetite
- Nausea and vomiting
- Fever and chills
- Abdominal bloating or swelling
- Pain worsening with movement, coughing, or deep breaths
If you or someone you know experiences these symptoms, seek immediate medical attention to avoid complications.
Causes of Appendicitis
Appendicitis usually results from a blockage in the appendix. Common causes include:
- Hardened stool (fecalith)
- Enlarged lymphoid follicles
- Parasitic or bacterial infections
- Trauma or foreign bodies
This blockage can cause bacterial overgrowth, leading to inflammation, infection, and potential rupture.
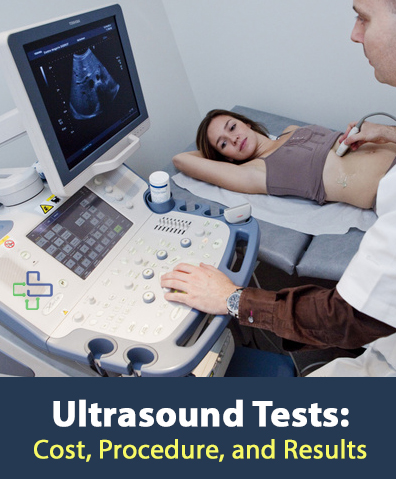
Diagnosis and Evaluation
Doctors diagnose appendicitis based on physical examination, symptoms, and diagnostic tests like:
- Blood tests to detect infection
- Urine tests to rule out urinary infections
- Abdominal ultrasound or CT scan to confirm inflammation
Quick diagnosis ensures timely surgery and minimizes the risk of complications.
Appendicitis Surgery in India
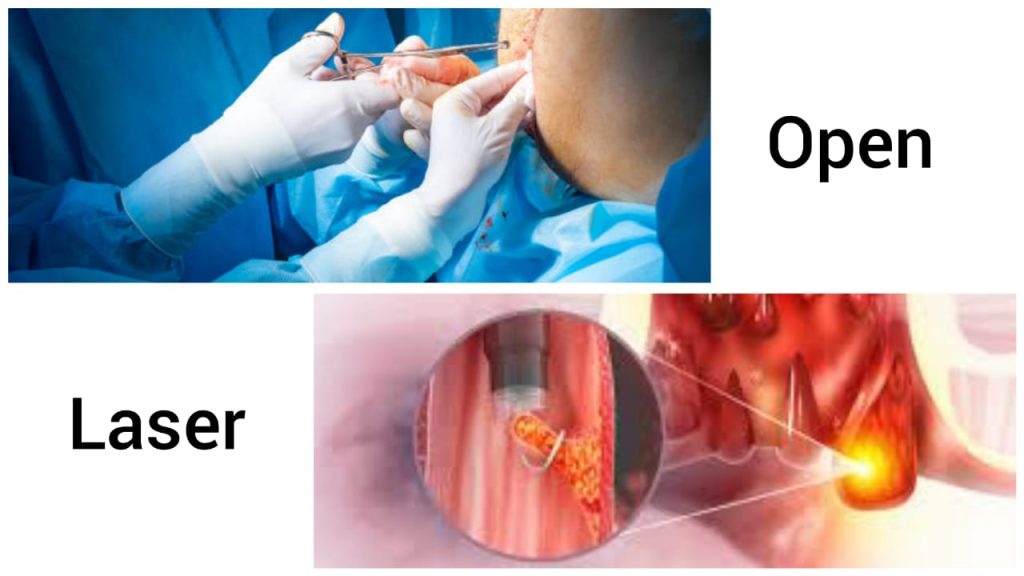
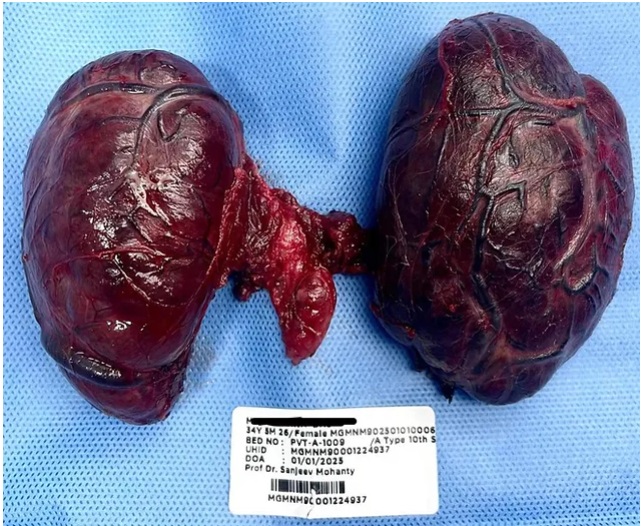
The most effective treatment for appendicitis is appendectomy—the surgical removal of the appendix. In India, two main surgical options are available:
- Laparoscopic Appendectomy
This is a minimally invasive surgery performed through small incisions using a camera and special instruments. It offers faster recovery, less pain, and minimal scarring. Patients can usually go home within 24–48 hours. - Open Appendectomy
In cases where the appendix has ruptured or if laparoscopy is not possible, open surgery is performed. This involves a larger incision and may require a longer hospital stay.
Recovery After Surgery
Most patients recover within 1–3 weeks after laparoscopic surgery. Post-surgery care includes:
- Taking prescribed antibiotics and pain relievers
- Avoiding strenuous activities for a few weeks
- Maintaining a light diet initially
- Attending follow-up appointments
Cost of Appendicitis Surgery in India
The cost of appendicitis surgery in India is affordable compared to many other countries. On average,Costs may vary depending on the hospital, city, and complexity of the case.
Conclusion
Appendicitis requires immediate medical attention. With advancements in surgical care, appendicitis surgery in India is both safe and affordable. If you or a loved one experiences symptoms of appendicitis, consult a healthcare provider immediately. Early diagnosis and timely surgery can prevent serious health risks and ensure a smooth recovery.
Don’t ignore signs of appendicitis. Early consultation with a specialist can save you from complications. Book your appointment today for appendicitis and take the first step towards safe and effective treatment